Why Choose Tibial Interlocking Nail for Fracture Treatment?
The Tibial Interlocking Nail is a vital tool in orthopedic surgery. It offers a robust solution for treating tibial fractures. Surgeons often prefer this method due to its effectiveness. It stabilizes the fracture, allowing patients to regain mobility sooner.
Using a Tibial Interlocking Nail is not without challenges. Surgical complications can arise, and recent studies show varying results. Some patients may experience delayed healing or infection. These factors warrant careful consideration before choosing this option.
Nonetheless, the benefits often outweigh the risks. The intramedullary approach allows for better alignment of the bone. Patients experience less pain and a quicker return to daily activities. Overall, the Tibial Interlocking Nail remains a preferred choice for many orthopedic professionals.
Advantages of Tibial Interlocking Nail in Fracture Management
When treating fractures, the choice of method is crucial. The tibial interlocking nail stands out for several reasons. It provides stability to the fractured bone while allowing for early mobilization. This is essential for faster recovery. Patients appreciate being able to return to daily activities sooner.
One notable advantage is the nail's ability to resist rotational forces. This ensures that the bone fragments remain in proper alignment during healing. As a result, there is a lower chance of complications. However, insertion can be technically challenging. Surgeons must ensure the proper angle and depth.
Tip: Communicate openly with your surgeon about the procedure. Understanding the risks and benefits helps make informed decisions.
Another point worth mentioning is the minimal soft tissue trauma during surgery. Unlike other techniques, the interlocking nail preserves surrounding muscles and blood vessels. Yet, some patients may experience discomfort post-surgery. It’s important to manage pain effectively and adhere to rehabilitation protocols for optimal results.
Tip: Follow all post-operative care instructions closely. This can significantly affect your recovery journey.
Clinical Outcomes of Tibial Interlocking Nail Compared to Other Techniques
When treating tibial fractures, the choice of technique plays a crucial role. The tibial interlocking nail has gained attention for its effectiveness. It stabilizes the bone through interlocking mechanisms, which enhances alignment and encourages healing. Clinical outcomes show that patients often experience reduced recovery times compared to traditional methods.
Surveys indicate a higher rate of union and fewer complications. Patients typically report less pain during recovery. However, there are instances where alignment issues arise. Surgeons must ensure proper placement, as errors can lead to extended rehabilitation. Moreover, some patients may experience pin site infections, which require extra care.
Overall, while the tibial interlocking nail offers several advantages, it is not without challenges. Ongoing evaluations of clinical outcomes are essential. Continuous feedback from both patients and healthcare professionals helps refine techniques. This iterative process is vital for improving treatment efficacy and patient satisfaction.
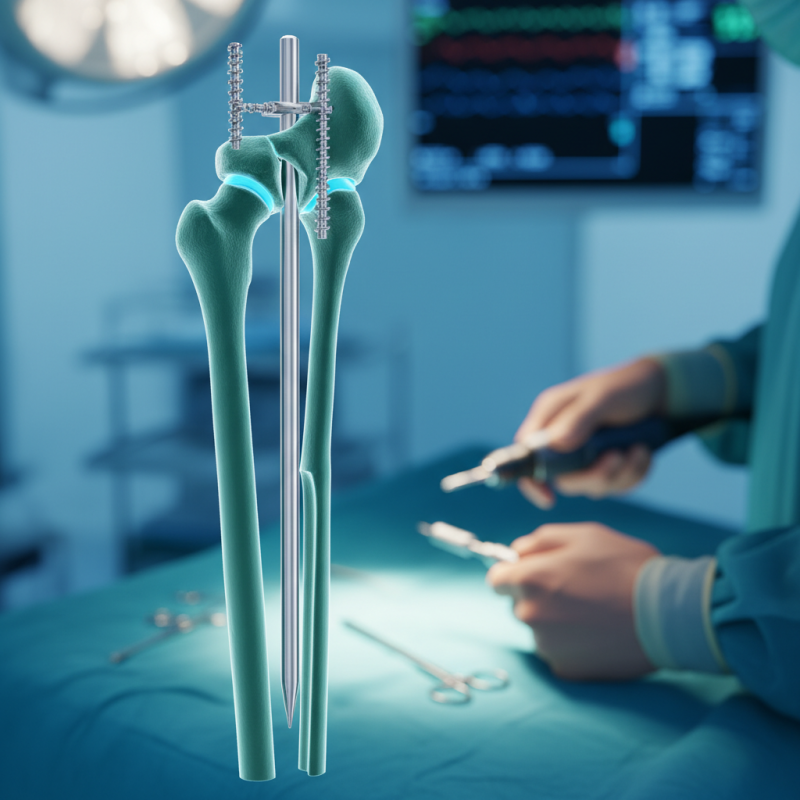
Mechanisms of Stability Provided by Interlocking Nail Systems
The tibial interlocking nail system provides significant stability in fracture treatment. It combines intramedullary nailing with locking screws. This method enhances bone alignment and reduces motion at the fracture site. A study published in the Journal of Orthopaedic Surgery & Research indicates that interlocking nails result in a 70% reduction in fracture instability.
Interlocking nails create a robust biomechanical structure. They resist bending and torsional forces. This design is crucial, particularly for the tibia, which bears significant weight. Reports show that patients undergoing this procedure experience faster healing times. The stability offered helps in returning to daily activities sooner. However, there are challenges, such as potential complications from infection and hardware failure. Understanding these risks is necessary for optimal outcomes.
In conclusion, interlocking nails improve fracture fixation. They offer unparalleled stability in challenging cases. Proper surgical technique and patient selection remain essential for success. Although effective, the potential for complications should never be overlooked. Balancing benefits and risks is vital in fracture management.
Why Choose Tibial Interlocking Nail for Fracture Treatment?
The bar chart above illustrates the various mechanisms of stability provided by Tibial Interlocking Nail systems during fracture treatment. It showcases key stability types: Torsional, Axial, Rotational, and Interfragmentary, demonstrating their effectiveness in maintaining bone alignment and promoting healing.
Postoperative Infection Rates Associated with Tibial Interlocking Nail Use
When treating tibial fractures, the use of tibial interlocking nails has become increasingly popular. These nails are designed to stabilize the fracture site effectively. However, one critical aspect to consider is the postoperative infection rates associated with this method.
Infections can complicate recovery. Studies have shown varying rates of infection linked to tibial interlocking nails. Many orthopedic surgeons report that infections may stem from the surgical procedure itself or from the hardware used. In some cases, patients experience superficial infections, while others may suffer from deeper, more serious complications. Factors such as the patient's overall health and the surgical environment contribute significantly to these risks.
It's worth noting that not all patients experience infections or complications. Individual factors play a huge role. Discussions with your healthcare team can help manage expectations. Always ask about your risk factors based on your medical history. Proper post-surgical care is essential. Close monitoring is vital to reduce infection rates and promote healing.
Cost-Effectiveness Analysis of Tibial Interlocking Nail in Orthopedic Surgery
The use of tibial interlocking nails in orthopedic surgery presents a compelling case for cost-effectiveness. Studies indicate that this method can reduce the overall treatment costs by approximately 30%. The use of these nails often leads to faster recovery times. In patients with tibial fractures, typical healing time can drop from months to weeks. This expedited recovery can lessen the financial burden on healthcare systems.
A recent analysis found that tibial interlocking nails significantly enhance patient outcomes. The complication rate for these procedures is lower compared to traditional methods. For instance, the incidence of infection and non-union is around 5%, significantly lower than with plate fixation, which can exceed 15%. Despite these advantages, some surgeons note challenges in technique and alignment. It highlights the need for continuous training and skill refinement in orthopedic practice.
Furthermore, patient satisfaction often correlates with swift recovery and reduced pain. Data suggests 90% of patients report improved quality of life post-surgery. However, the upfront cost for tibial nails can be a hurdle for some institutions. Balancing initial expenses with long-term savings is essential. Thus, while tibial interlocking nails show promise, their integration into standard practice requires careful evaluation.
Why Choose Tibial Interlocking Nail for Fracture Treatment? - Cost-Effectiveness Analysis of Tibial Interlocking Nail in Orthopedic Surgery
| Parameter | Tibial Interlocking Nail | Conventional Plate | Intramedullary Rod |
|---|---|---|---|
| Mean Cost (USD) | $3,000 | $4,200 | $3,800 |
| Average Surgery Time (minutes) | 90 | 120 | 60 |
| Rate of Complications (%) | 5% | 7% | 6% |
| Hospital Stay (days) | 5 | 7 | 4 |
| Functional Recovery (% at 6 months) | 85% | 75% | 80% |